Beyond the DASH-Sodium Trial
 The DASH-Sodium trial showed that salt restriction, coupled with the DASH diet, reduced blood pressure (BP) in those with Stage 1 hypertension (HTN) as much as or more than does any single anti-HTN drug. Drugs used to treat HTN can cause a variety of adverse side effects and increase the risk of Type 2 diabetes and possibly heart disease. By contrast, reducing salt intake appears to reduce the incidence of stroke, heart disease, osteoporosis, kidney stones, stomach cancer, dementia and headaches.
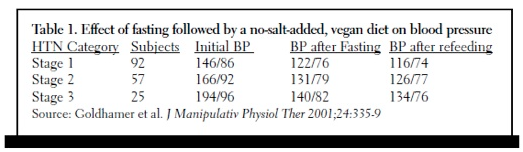
The DASH-Sodium trial showed that salt restriction, coupled with the DASH diet, reduced blood pressure (BP) in those with Stage 1 hypertension (HTN) as much as or more than does any single anti-HTN drug. Drugs used to treat HTN can cause a variety of adverse side effects and increase the risk of Type 2 diabetes and possibly heart disease. By contrast, reducing salt intake appears to reduce the incidence of stroke, heart disease, osteoporosis, kidney stones, stomach cancer, dementia and headaches.The DASH-Sodium trial clearly showed that reducing dietary sodium from salt to about 1500 mg daily is both safe and effective for treating most people with Stage 1 HTN. However, important questions remain. Would even greater reductions in salt intake be even more effective at lowering BP, and can an even lower-salt diet be effective in treating those with Stage 2 and 3 HTN? A recent study of 174 patients with varying degrees of HTN suggests the answer to both of these questions is yes. Table 1 above summarizes the results. These patients were placed on a low-fat, no-added-salt, vegan diet for about 3 days. They then fasted with distilled water only for an average of about 11 days and were then placed back on the same vegan diet for about another week. Average weight loss was nearly 15 pounds over an average of 20 days. Only 11 of these 174 patients were on anti-hypertensive drugs initially, and by the end of the study all had been taken off all BP medications. The average drop in BP was 37/13, but for those with the Stage 3 HTN, the average drop was a remarkable 60/17. Nearly 90% of all HTN patients were able to attain a BP of less than 140/90 with diet alone in an average of about 20 days.Bottom Line: The results of this study suggest that purging the body of excess salt is often necessary in order to control HTN. It also suggests that the nearly 4 grams of salt (1500 mg sodium) used in the DASH-sodium study is still excessive for optimal medical nutritional therapy of hypertension.


