IOM 2013 Report on Sodium Intake
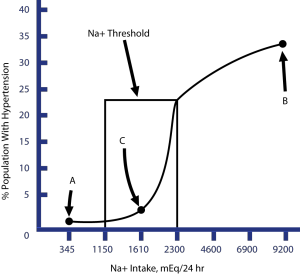 The Institute of Medicine (IOM) issued a report, commissioned by the CDC, in May 2013. This report set out to evaluate data from outcome studies published since the IOM's 2004 report on water and electrolytes, which included the need for salt. The earlier report suggested no more than 1,200 to 1,500 mg of sodium were needed by virtually all Americans. This new IOM report focused on studies that attempted to link salt/sodium intake with health outcome data like cardiovascular disease (CVD) events and total mortality. This new IOM report largely ignored the now well-established impact of salt reduction on lowering blood pressure (BP) and focused instead on clinical trials and observation studies that examined the direct correlation between salt intake and outcome data on the number of heart attacks, strokes, heart failure hospitalizations, and deaths. The new IOM report noted that there were many weaknesses with all the studies they examined and so making any firm conclusions based on this newer data was not possible (1). Unfortunately, some media reports about the new IOM Report grossly misrepresented what the IOM Report actually concluded. These seriously biased or naïve media reports could easily mislead Americans into believing that reducing salt/sodium intake probably won't help prevent heart disease or stroke and may even increase the risk of dying.New York Times Misinterprets New IOM ReportOne of the more egregious articles on the new IOM Report was penned by Gina Kolata for the New York (NY) Times (2). The article by Ms Kolata and the accompanying editorial by the NY Times editorial staff claimed the IOM Report said that not only was there was no benefit from reducing salt intake to the 1500mg sodium/day level but that such a reduction could be dangerous. This despite the fact that the 1,500 mg sodium/day maximum level is now recommended by the American Heart Association and the latest US Dietary Guidelines. The American Heart Association has already said that the new studies do not undermine their advice to limit sodium intake to no more than 1,500 mg/day.Where did the NY Times and other media reports go wrong? Put simply, the new IOM report did not conclude a 1500mg sodium per day goal has no proven health benefits and indeed has potential health risks, as Ms Kolata implied. Rather, the IOM report simply stated that the evidence we currently have from direct health outcomes studies is way too flawed and insufficient to make any new recommendations at all. It concluded that more and better quality studies, which look at salt intake and health outcomes, is needed.Contrary to many media reports, there is strong evidence demonstrating beyond any reasonable doubt that reducing sodium intake from below 2,300 mg/day down to below 1,500mg/day reduces BP in the short-term and likely also prevents the development of hypertension (HTN) over a lifetime. For example, the DASH-Sodium Trial showed a greater fall in BP when sodium intake was reduced from about 2,400 mg to 1,500 mg per day than when it was reduced from about 3,300 mg down to 2,400 mg/day. This was true both on a typical American diet and on a healthier DASH-diet (3).Studies of human populations consuming a diet averaging less than 50mmol of salt (or <1,150 mg Na+) per day see little or no rise in BP with age and HTN is rare even on older individuals. By contrast, all human populations averaging 100 mmol of salt (>2,300 mg Na+) daily experience increasing BP with age with the majority of people in those populations developing HTN by the time they reach their 60s. For example, the large Intersalt study examined the relationship between 24-hour urinary salt excretion and BP in 52 population groups of people between the ages of 20 and 59 around the world. Only 4 of these populations consumed less than 50 mmol of salt a day and the other 48 averaged more than 100 mmol of salt daily. In only the 4 consuming diets with little or no added salt did BP not increase with age and HTN was rarely observed. Across the other 48 salt-adding populations, sodium was significantly related to the rise of BP with age, not to median BP or prevalence of HTN (4). The results of this study comport precisely with the earlier hypothesis of the relationship between the incidence of HTN and the average salt intake. The figure below shows the hypothesized relationship between the average daily salt intake of a population group and the incidence of HTN. As you can see, with about 70 mmol of salt (or 1,600 mg sodium) per day, the incidence of HTN is very low. As salt intake rises up to around 2,300 mg of sodium per day (or 100 mmol salt) a large percentage of the population will develop HTN. Above and below the "threshold level" further reductions or increases in median salt intake has a relatively modest impact on BP. Given the difficulty in measuring salt intake over a lifetime and other dietary and lifestyle factors influencing BP, the modest predicted changes in BP outside the "threshold level" can obscure the independent effects of dietary salt intake.Bottom Line: There is very good quality research from the DASH-Sodium Trial and others demonstrating that reducing sodium to about 1,500 mg/day from 2,300+ mg/day significantly lowers BP, especially in those with HTN. And no one questions the overwhelming data showing that elevated BP is the #1 risk factor for CVD accounting for about half of all CVD events. So would reducing all Americans sodium intake to less than 1500mg per day prevent all hypertension? Probably not but it would certainly prevent the vast majority of primary HTN and nothing in the recent IOM Report undermines these facts.Sources:
The Institute of Medicine (IOM) issued a report, commissioned by the CDC, in May 2013. This report set out to evaluate data from outcome studies published since the IOM's 2004 report on water and electrolytes, which included the need for salt. The earlier report suggested no more than 1,200 to 1,500 mg of sodium were needed by virtually all Americans. This new IOM report focused on studies that attempted to link salt/sodium intake with health outcome data like cardiovascular disease (CVD) events and total mortality. This new IOM report largely ignored the now well-established impact of salt reduction on lowering blood pressure (BP) and focused instead on clinical trials and observation studies that examined the direct correlation between salt intake and outcome data on the number of heart attacks, strokes, heart failure hospitalizations, and deaths. The new IOM report noted that there were many weaknesses with all the studies they examined and so making any firm conclusions based on this newer data was not possible (1). Unfortunately, some media reports about the new IOM Report grossly misrepresented what the IOM Report actually concluded. These seriously biased or naïve media reports could easily mislead Americans into believing that reducing salt/sodium intake probably won't help prevent heart disease or stroke and may even increase the risk of dying.New York Times Misinterprets New IOM ReportOne of the more egregious articles on the new IOM Report was penned by Gina Kolata for the New York (NY) Times (2). The article by Ms Kolata and the accompanying editorial by the NY Times editorial staff claimed the IOM Report said that not only was there was no benefit from reducing salt intake to the 1500mg sodium/day level but that such a reduction could be dangerous. This despite the fact that the 1,500 mg sodium/day maximum level is now recommended by the American Heart Association and the latest US Dietary Guidelines. The American Heart Association has already said that the new studies do not undermine their advice to limit sodium intake to no more than 1,500 mg/day.Where did the NY Times and other media reports go wrong? Put simply, the new IOM report did not conclude a 1500mg sodium per day goal has no proven health benefits and indeed has potential health risks, as Ms Kolata implied. Rather, the IOM report simply stated that the evidence we currently have from direct health outcomes studies is way too flawed and insufficient to make any new recommendations at all. It concluded that more and better quality studies, which look at salt intake and health outcomes, is needed.Contrary to many media reports, there is strong evidence demonstrating beyond any reasonable doubt that reducing sodium intake from below 2,300 mg/day down to below 1,500mg/day reduces BP in the short-term and likely also prevents the development of hypertension (HTN) over a lifetime. For example, the DASH-Sodium Trial showed a greater fall in BP when sodium intake was reduced from about 2,400 mg to 1,500 mg per day than when it was reduced from about 3,300 mg down to 2,400 mg/day. This was true both on a typical American diet and on a healthier DASH-diet (3).Studies of human populations consuming a diet averaging less than 50mmol of salt (or <1,150 mg Na+) per day see little or no rise in BP with age and HTN is rare even on older individuals. By contrast, all human populations averaging 100 mmol of salt (>2,300 mg Na+) daily experience increasing BP with age with the majority of people in those populations developing HTN by the time they reach their 60s. For example, the large Intersalt study examined the relationship between 24-hour urinary salt excretion and BP in 52 population groups of people between the ages of 20 and 59 around the world. Only 4 of these populations consumed less than 50 mmol of salt a day and the other 48 averaged more than 100 mmol of salt daily. In only the 4 consuming diets with little or no added salt did BP not increase with age and HTN was rarely observed. Across the other 48 salt-adding populations, sodium was significantly related to the rise of BP with age, not to median BP or prevalence of HTN (4). The results of this study comport precisely with the earlier hypothesis of the relationship between the incidence of HTN and the average salt intake. The figure below shows the hypothesized relationship between the average daily salt intake of a population group and the incidence of HTN. As you can see, with about 70 mmol of salt (or 1,600 mg sodium) per day, the incidence of HTN is very low. As salt intake rises up to around 2,300 mg of sodium per day (or 100 mmol salt) a large percentage of the population will develop HTN. Above and below the "threshold level" further reductions or increases in median salt intake has a relatively modest impact on BP. Given the difficulty in measuring salt intake over a lifetime and other dietary and lifestyle factors influencing BP, the modest predicted changes in BP outside the "threshold level" can obscure the independent effects of dietary salt intake.Bottom Line: There is very good quality research from the DASH-Sodium Trial and others demonstrating that reducing sodium to about 1,500 mg/day from 2,300+ mg/day significantly lowers BP, especially in those with HTN. And no one questions the overwhelming data showing that elevated BP is the #1 risk factor for CVD accounting for about half of all CVD events. So would reducing all Americans sodium intake to less than 1500mg per day prevent all hypertension? Probably not but it would certainly prevent the vast majority of primary HTN and nothing in the recent IOM Report undermines these facts.Sources:
- Institute of Medicine. 2013 Sodium Intake in Populations: Assessment of Evidence. Washington, DC: the National Academies Press, May 14, 2013.
- Kolata G. No benefit seen in sharp limits on salt in diet. NY Times May 14, 2013.
- Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med 2001;344:3-10.
- Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988; 297: 319–328.
By James J. Kenney, PhD, FACN


