A Better Way to Lend a Hand to Diabetes Patients
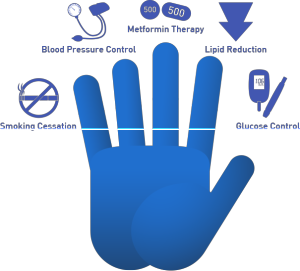 An editorial in a February issue of American Family Physician proposed a simple way for physicians to communicate treatment priorities for patients with type 2 diabetes. Their "hand" illustration re-prioritizes treatment goals. It conveys that glycemic control or blood sugar (BS) control is no longer the top priority. The new medical treatment priority model illustrates that glucose control is not as important as smoking cessation, blood pressure (BP) control, use of metformin, and lipid control. Take a look at the full press release.This proposed change of the treatment goal priorities for people with diabetes, while it may be a step in the right direction, is not optimal. This revised largely medical/ pharmaceutical approach, called "lending a finger," (see Figure 1) still misses the two most important priorities for reducing morbidity and mortality in people with type 2 diabetes. It is overly MD-centric, which may enable those with type 2 diabetes to believe that they require prescription drugs to control not only their BS but also their BP and blood lipids.On the plus side, it's nice to see MDs recognize that their all-too-myopic focus on controlling BS has too often done more harm than good for many people with diabetes. This focus has led to unproductive emphasizing of the diet's glycemic index (GI) and glycemic load (GL) as well as a sometimes obsessive focus on counting grams of carbohydrate to control BS. Of course, counting grams of carbohydrate is most counterproductive for those with type 2 diabetes, especially if it leads them to reduce their intake of high-carbohydrate whole plant foods. Indeed, even for type 1 diabetes patients, where arguably counting grams of carbohydrate may have some limited utility, at least for BS control, a systematic analysis of the best data available suggests it is still pretty close to useless, even for improving BS control (1). The ACCORD studies showed that aggressively lowering BS levels with diabetes medications achieved increased overall mortality. As a result of this data, the American Diabetes Association apparently has realized that their obsessive BS focus was not all that beneficial for people with diabetes, especially those with type 2 diabetes (2).
An editorial in a February issue of American Family Physician proposed a simple way for physicians to communicate treatment priorities for patients with type 2 diabetes. Their "hand" illustration re-prioritizes treatment goals. It conveys that glycemic control or blood sugar (BS) control is no longer the top priority. The new medical treatment priority model illustrates that glucose control is not as important as smoking cessation, blood pressure (BP) control, use of metformin, and lipid control. Take a look at the full press release.This proposed change of the treatment goal priorities for people with diabetes, while it may be a step in the right direction, is not optimal. This revised largely medical/ pharmaceutical approach, called "lending a finger," (see Figure 1) still misses the two most important priorities for reducing morbidity and mortality in people with type 2 diabetes. It is overly MD-centric, which may enable those with type 2 diabetes to believe that they require prescription drugs to control not only their BS but also their BP and blood lipids.On the plus side, it's nice to see MDs recognize that their all-too-myopic focus on controlling BS has too often done more harm than good for many people with diabetes. This focus has led to unproductive emphasizing of the diet's glycemic index (GI) and glycemic load (GL) as well as a sometimes obsessive focus on counting grams of carbohydrate to control BS. Of course, counting grams of carbohydrate is most counterproductive for those with type 2 diabetes, especially if it leads them to reduce their intake of high-carbohydrate whole plant foods. Indeed, even for type 1 diabetes patients, where arguably counting grams of carbohydrate may have some limited utility, at least for BS control, a systematic analysis of the best data available suggests it is still pretty close to useless, even for improving BS control (1). The ACCORD studies showed that aggressively lowering BS levels with diabetes medications achieved increased overall mortality. As a result of this data, the American Diabetes Association apparently has realized that their obsessive BS focus was not all that beneficial for people with diabetes, especially those with type 2 diabetes (2).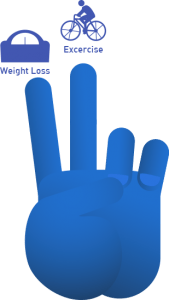 From my perspective, this new proposed "lending a finger" proposal is not all that much better than the prior myopic focus on BS control, carbohydrate counting, and glycemic load. Indeed the "hand" actually missed the two most important factors for not only improving and reversing insulin resistance (and associated metabolic ills), but also increasing longevity in people with type 2 diabetes and the metabolic syndrome. My "lending a finger" hand (see Figure 2) would look like the two finger peace sign.Index finger: "Weight loss" ?This would be achieved not by calorie counting but by changing what people with type 2 diabetes are told to eat. Rather than focus on counting grams of carbohydrate, patients should shift their focus to eating less processed foods with lower calorie density and higher fiber content. That diet would be composed largely of whole grains, fruits, and vegetables, with marked reductions in salt, sugar-rich drinks, and fatty animal products.Middle finger: "Exercise" ?This would consist of at least one hour of daily aerobic exercise, with additional resistance training 2-3 times per week. It would also discourage long periods of sitting.As shown in the DPPT trail (see Figure 3), those two lifestyle changes and a very modest weight loss reduced insulin resistance and were far more effective than metformin for preventing people with pre-diabetes from progressing to type 2 diabetes over several years. A healthful diet & exercise program has been shown to eliminate the need for any diabetes medication to control BS in most people recently diagnosed with type 2 diabetes. A healthful diet and regular exercise can also eliminate hypertension and dyslipidemia in most people, so there goes the need for MDs and pharmaceutical agents to control BP and blood lipids too. Once one realizes that type 2 diabetes is largely caused by excessive weight gain brought on by the typical American diet and inactivity, the obvious way to stop and prevent type 2 diabetes is by eliminating the poor diet and inactivity that caused the weight gain, insulin resistance, and associated metabolic abnormalities. Sadly, in the USA, type 2 diabetes is viewed as a medical problem when in fact it is caused largely by poor diet and lifestyle choices. Improving the diet and beginning regular exercise can dramatically reduce or eliminate the need for MDs and pharmaceutical agents to prevent or treat type 2 diabetes patients who still have enough beta-cell function to produce sufficient insulin, once their insulin sensitivity is enhanced by a healthful diet and exercise program, with a sufficient loss of abdominal fat stores.
From my perspective, this new proposed "lending a finger" proposal is not all that much better than the prior myopic focus on BS control, carbohydrate counting, and glycemic load. Indeed the "hand" actually missed the two most important factors for not only improving and reversing insulin resistance (and associated metabolic ills), but also increasing longevity in people with type 2 diabetes and the metabolic syndrome. My "lending a finger" hand (see Figure 2) would look like the two finger peace sign.Index finger: "Weight loss" ?This would be achieved not by calorie counting but by changing what people with type 2 diabetes are told to eat. Rather than focus on counting grams of carbohydrate, patients should shift their focus to eating less processed foods with lower calorie density and higher fiber content. That diet would be composed largely of whole grains, fruits, and vegetables, with marked reductions in salt, sugar-rich drinks, and fatty animal products.Middle finger: "Exercise" ?This would consist of at least one hour of daily aerobic exercise, with additional resistance training 2-3 times per week. It would also discourage long periods of sitting.As shown in the DPPT trail (see Figure 3), those two lifestyle changes and a very modest weight loss reduced insulin resistance and were far more effective than metformin for preventing people with pre-diabetes from progressing to type 2 diabetes over several years. A healthful diet & exercise program has been shown to eliminate the need for any diabetes medication to control BS in most people recently diagnosed with type 2 diabetes. A healthful diet and regular exercise can also eliminate hypertension and dyslipidemia in most people, so there goes the need for MDs and pharmaceutical agents to control BP and blood lipids too. Once one realizes that type 2 diabetes is largely caused by excessive weight gain brought on by the typical American diet and inactivity, the obvious way to stop and prevent type 2 diabetes is by eliminating the poor diet and inactivity that caused the weight gain, insulin resistance, and associated metabolic abnormalities. Sadly, in the USA, type 2 diabetes is viewed as a medical problem when in fact it is caused largely by poor diet and lifestyle choices. Improving the diet and beginning regular exercise can dramatically reduce or eliminate the need for MDs and pharmaceutical agents to prevent or treat type 2 diabetes patients who still have enough beta-cell function to produce sufficient insulin, once their insulin sensitivity is enhanced by a healthful diet and exercise program, with a sufficient loss of abdominal fat stores.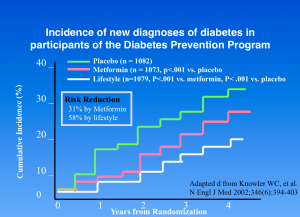 Behavioral/psychology health professionals playing a more prominent role to help with smoking cessation and with getting people with insulin resistance and/or type 2 diabetes to accept that their disease was largely brought on by their diet and lifestyle choices rather than "bad genes" is a great first step. Helping patients realize that, in order to reverse their illness (or at least to markedly improve their health outcomes), they must accept personal responsibility for their illness and then stop the self-destructive behaviors that make their disease worse over time (despite all the prescription drugs they take, all the carb counting, and BS monitoring efforts). We know that most type 2 diabetics who are undergoing traditional medical therapy will ultimately end up with all sorts of serious ills such as neuropathy, failing kidneys, (which, when they fail means that patients must spend the rest of their lives on dialysis), a markedly elevated risk of retinal damage, a higher risk of cataracts destroying their vision, a marked increase in dementia, stroke, heart attack, and heart failure, and all those unpleasant drug side effects that undermine their quality of life.Bottom Line: It is time to recognize what causes diabetes and discourage the behaviors that promote it. It is increasingly clear that adopting a more healthful diet and lifestyle can help reverse the disease. So rather than relying on a medical approach to control risk factors with drugs and/or surgery it would be better for people with the metabolic syndrome or type 2 DM to be encouraged to change what they eat and become less sedentary. This is not to say that drugs and surgeries have no benefits, but the medical approach certainly won't stop the progression of most of the ills that people with type 2 diabetes must deal with sooner or later. Perhaps it is time for healthcare providers to stop being enablers of an unhealthful disease-promoting diet and lifestyle and educate people, empowering them to reverse those harmful behaviors.References:
Behavioral/psychology health professionals playing a more prominent role to help with smoking cessation and with getting people with insulin resistance and/or type 2 diabetes to accept that their disease was largely brought on by their diet and lifestyle choices rather than "bad genes" is a great first step. Helping patients realize that, in order to reverse their illness (or at least to markedly improve their health outcomes), they must accept personal responsibility for their illness and then stop the self-destructive behaviors that make their disease worse over time (despite all the prescription drugs they take, all the carb counting, and BS monitoring efforts). We know that most type 2 diabetics who are undergoing traditional medical therapy will ultimately end up with all sorts of serious ills such as neuropathy, failing kidneys, (which, when they fail means that patients must spend the rest of their lives on dialysis), a markedly elevated risk of retinal damage, a higher risk of cataracts destroying their vision, a marked increase in dementia, stroke, heart attack, and heart failure, and all those unpleasant drug side effects that undermine their quality of life.Bottom Line: It is time to recognize what causes diabetes and discourage the behaviors that promote it. It is increasingly clear that adopting a more healthful diet and lifestyle can help reverse the disease. So rather than relying on a medical approach to control risk factors with drugs and/or surgery it would be better for people with the metabolic syndrome or type 2 DM to be encouraged to change what they eat and become less sedentary. This is not to say that drugs and surgeries have no benefits, but the medical approach certainly won't stop the progression of most of the ills that people with type 2 diabetes must deal with sooner or later. Perhaps it is time for healthcare providers to stop being enablers of an unhealthful disease-promoting diet and lifestyle and educate people, empowering them to reverse those harmful behaviors.References:
- Bell KJ, et al. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. The Lancet Diabetes & Endocrinology. doi:10.1016/S2213-8587 (13)70144-X.
- The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008; 358: 2545–2559
By James J. Kenney, PhD, FACNPostscript: A study released after this article was written supports its conclusion that it would be far better for people with type 2 DM to lose weight and exercise to control or even largely eliminate their disease than to simply take multiple drugs to control its varied metabolic problems. This new study proves type 2 DM is largely caused by an unhealthy diet and lifestyle that leads to an increased accumulation of body fat. This research published in the Feb. 6 issue of the American Journal of Human Genetics, Dr. Keating and V. Holmes, M.D., Ph.D., of the Perelman School of Medicine at the University of Pennsylvania used a recently developed epidemiology tool called Mendelian randomization (MR) that rules out confounding factors such as behavioral and environmental influences to construct genetic risk scores for specific traits of interest. The study team analyzed eight population groups including over 34,000 individuals of European descent, of whom over 4,400 had type 2 diabetes.Their analysis demonstrated the causal relationship between increasing BMI in promoting insulin resistance and other metabolic abnormalities that markedly increase the risk of developing type 2 DM. "Our findings suggest that lowering BMI is likely to result in multiple reductions of cardiovascular traits: in blood pressure, inflammation, fasting glucose and insulin, and in the risk of type 2 diabetes," said Dr. Keating. By James J. Kenney, PhD, FACN"Causal Effects of Body Mass Index on Cardiometabolic Traits and Events: A Mendelian Randomization Analysis," American Journal of Human Genetics, published online Jan. 23, 2014 and in print Feb. 6, 2014. doi.10.1016/j.ajhg.2013.12.014
