Is Being Overweight Healthier?
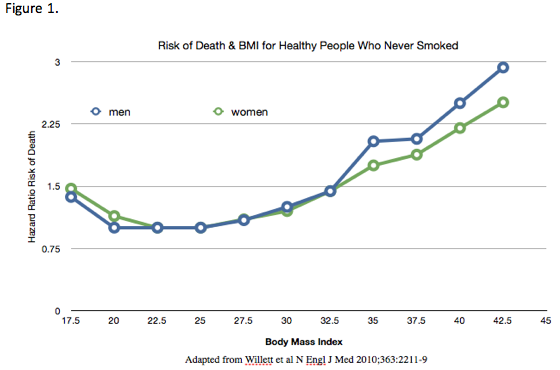 On January 2nd, just in time to damper the enthusiasm of many overweight people's New Year's resolutions to eat healthier, exercise more, and lose excess body weight, we have the Journal of the American Medical Association publish yet another seriously flawed study from Dr. Flegal and her associates at the Center for Disease Control.1 Flegal's study certainly got a lot of press. While some of the press coverage pointed out some of the reasons the study's data was misleading, many presented the data with little criticism, suggesting this study showed being overweight actually helped reduce the risk of dying. In too many cases the media, along with the study's authors, failed to understand that correlation should not be confused with causation.Critics of this study focused on some of the questionable methods Flegal used in compiling statistics from previous studies. For example, Flegal included people too thin to fit what most consider to be normal weight range (BMI 20 to 24.9). Many of these ultra thin individuals were likely already somewhat emaciated by cancer or other serious disease at the time their BMI was measured. She also included smokers, who tend to be thinner but who have a much greater risk of dying from heart disease, emphysema, and cancer than nonsmokers. The statistical associations created by this study's inclusion of smokers and people with pre-existing illnesses was likely largely responsible for producing questionable correlations between lower BMI and an increased risk of dying.One of Flegal's most vocal critics was Dr. Walter Willett of the Harvard School of Public Health. He claimed that Flegal's study was "an even greater pile of rubbish" than Flegal's 2005 study. Willett and others have done research since the 2005 study that eliminated most of the questionable correlations between lower BMI and an increased risk of dying. In a 2010 study, Willett did a meta-analysis of several large studies that looked at people who never smoked. He also looked at the deaths that occurred in the first few years after BMI was measured, eliminating data from those subjects in order to get rid of data from people whose low BMI was likely caused by some serious illnesses that had already caused them to lose a lot of weight. Data from Willett's 2010 study is shown in Figure 1.Willett's data indicate that the risk of death was significantly greater in people whose initial BMIs put them in the overweight (25 to 29.9) and obese (30 or greater) categories, compared with those with normal weight BMIs (20 and 24.9). Even Willett's data found that the risk of dying for those who were very thin (BMI< 18) was higher even for people who appeared to be healthy nonsmokers.Flegal defended her work by claiming she used standard categories for weight classes and made some statistical adjustments for smokers, but she included data from studies that defined normal weight as being well below BMI of 20. Obviously not all people who become emaciated due to chronic ills are in hospitals or hospices as she assumed. Far more are in nursing homes and they were included in her study. A far better way to statistically correct for illnesses that lead to weight loss and then death is to wait several years after BMI is measured to start looking for deaths. Willett did that but Flegal did not. This statistical adjustment largely eliminates most of those whose sickness-caused weight loss lead to their deaths. Failure to note this creates a non-causal statistical correlation between lower BMI and increased mortality, which distracts from the biological reality of disease-related illness leading to weight loss and a greater risk of dying.Research in numerous animals shows a reduced calorie intake slows down the aging process, which suggests that eating more calories and gaining weight may actually cause people to age a bit faster. On the other hand, being very lean may not always improve survival. For example, older people with more body fat may survive a serious infection simply because their weight while sick is less likely to reach a critically low BMI level, leaving them better able to fight off the infection. However, being overweight or obese promotes many types of cancer, raises blood pressure, promotes type 2 diabetes, increases gallstones, osteoarthritis, senility, heart failure, and numerous other ills that can increase both morbidity and mortality. We all know people who were overweight or obese most of their lives, but unless they die suddenly from a heart attack or stroke, they typically lose a lot of weight before dying.Bottom Line: There is a big difference between losing weight unintentionally and intentionally. People with Alzheimer's, congestive heart failure, emphysema, renal failure, and numerous other ills often lose weight unintentionally for years before succumbing to their disease. Unintentional weight loss is often associated with serious disease that markedly increases the risk of dying. However, this is very different than healthy but overweight people intentionally losing weight by adopting a healthful diet and exercise program. This results in a marked improvement in numerous disease risk factors and ultimately reduces the risk of dying from many serious degenerative diseases. For most, this almost certainly increases longevity.By James J. Kenney PhD, FACN1. Flegal KM, et al. JAMA 2013;309: 71-82 or http://jama.jamanetwork. com/article.aspx?articleid=1555137
On January 2nd, just in time to damper the enthusiasm of many overweight people's New Year's resolutions to eat healthier, exercise more, and lose excess body weight, we have the Journal of the American Medical Association publish yet another seriously flawed study from Dr. Flegal and her associates at the Center for Disease Control.1 Flegal's study certainly got a lot of press. While some of the press coverage pointed out some of the reasons the study's data was misleading, many presented the data with little criticism, suggesting this study showed being overweight actually helped reduce the risk of dying. In too many cases the media, along with the study's authors, failed to understand that correlation should not be confused with causation.Critics of this study focused on some of the questionable methods Flegal used in compiling statistics from previous studies. For example, Flegal included people too thin to fit what most consider to be normal weight range (BMI 20 to 24.9). Many of these ultra thin individuals were likely already somewhat emaciated by cancer or other serious disease at the time their BMI was measured. She also included smokers, who tend to be thinner but who have a much greater risk of dying from heart disease, emphysema, and cancer than nonsmokers. The statistical associations created by this study's inclusion of smokers and people with pre-existing illnesses was likely largely responsible for producing questionable correlations between lower BMI and an increased risk of dying.One of Flegal's most vocal critics was Dr. Walter Willett of the Harvard School of Public Health. He claimed that Flegal's study was "an even greater pile of rubbish" than Flegal's 2005 study. Willett and others have done research since the 2005 study that eliminated most of the questionable correlations between lower BMI and an increased risk of dying. In a 2010 study, Willett did a meta-analysis of several large studies that looked at people who never smoked. He also looked at the deaths that occurred in the first few years after BMI was measured, eliminating data from those subjects in order to get rid of data from people whose low BMI was likely caused by some serious illnesses that had already caused them to lose a lot of weight. Data from Willett's 2010 study is shown in Figure 1.Willett's data indicate that the risk of death was significantly greater in people whose initial BMIs put them in the overweight (25 to 29.9) and obese (30 or greater) categories, compared with those with normal weight BMIs (20 and 24.9). Even Willett's data found that the risk of dying for those who were very thin (BMI< 18) was higher even for people who appeared to be healthy nonsmokers.Flegal defended her work by claiming she used standard categories for weight classes and made some statistical adjustments for smokers, but she included data from studies that defined normal weight as being well below BMI of 20. Obviously not all people who become emaciated due to chronic ills are in hospitals or hospices as she assumed. Far more are in nursing homes and they were included in her study. A far better way to statistically correct for illnesses that lead to weight loss and then death is to wait several years after BMI is measured to start looking for deaths. Willett did that but Flegal did not. This statistical adjustment largely eliminates most of those whose sickness-caused weight loss lead to their deaths. Failure to note this creates a non-causal statistical correlation between lower BMI and increased mortality, which distracts from the biological reality of disease-related illness leading to weight loss and a greater risk of dying.Research in numerous animals shows a reduced calorie intake slows down the aging process, which suggests that eating more calories and gaining weight may actually cause people to age a bit faster. On the other hand, being very lean may not always improve survival. For example, older people with more body fat may survive a serious infection simply because their weight while sick is less likely to reach a critically low BMI level, leaving them better able to fight off the infection. However, being overweight or obese promotes many types of cancer, raises blood pressure, promotes type 2 diabetes, increases gallstones, osteoarthritis, senility, heart failure, and numerous other ills that can increase both morbidity and mortality. We all know people who were overweight or obese most of their lives, but unless they die suddenly from a heart attack or stroke, they typically lose a lot of weight before dying.Bottom Line: There is a big difference between losing weight unintentionally and intentionally. People with Alzheimer's, congestive heart failure, emphysema, renal failure, and numerous other ills often lose weight unintentionally for years before succumbing to their disease. Unintentional weight loss is often associated with serious disease that markedly increases the risk of dying. However, this is very different than healthy but overweight people intentionally losing weight by adopting a healthful diet and exercise program. This results in a marked improvement in numerous disease risk factors and ultimately reduces the risk of dying from many serious degenerative diseases. For most, this almost certainly increases longevity.By James J. Kenney PhD, FACN1. Flegal KM, et al. JAMA 2013;309: 71-82 or http://jama.jamanetwork. com/article.aspx?articleid=1555137


