Digestive Diseases 101
May is Digestive Diseases Awareness Month. What do you know about digestive diseases?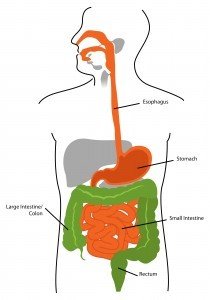 For a comprehensive rundown of digestive diseases, check out this A-Z list from the National Institute of Diabetes and Digestive and Kidney Diseases. Today, to help raise awareness of digestive diseases, we're going to zoom in on 5 conditions:
For a comprehensive rundown of digestive diseases, check out this A-Z list from the National Institute of Diabetes and Digestive and Kidney Diseases. Today, to help raise awareness of digestive diseases, we're going to zoom in on 5 conditions:
- Diverticular Disease
- Celiac Disease
- Crohn's Disease
- Gastroesophageal Reflux Disease
- Ulcerative Colitis
Diverticular Disease affects the colon, which is part of the large intestine. People get diverticular disease when small sacs are created in weak spots in the colon. These sacs push outward and are usually found in the lower colon, which is also known as the sigmoid colon. These pouches are called diverticula, and they are at the heart of diverticular disease.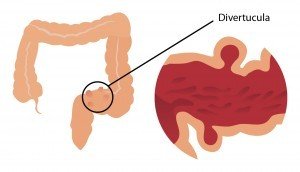 Diverticular disease occurs when the diverticula become irritated, swollen, or inflamed, which in turn leads to infection (diverticulitis) or when a blood vessel in a diverticulum bursts (diverticular bleeding). When the diverticula cause neither diverticulitis nor diverticular bleeding, the condition is called diverticulosis. The symptoms of diverticulosis include bloating, cramps in the lower abdomen, or pain in the lower abdomen. The symptoms of diverticular disease can be more severe. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "People with diverticulitis may have many symptoms, the most common of which is pain in the lower left side of the abdomen. The pain is usually severe and comes on suddenly, though it can also be mild and then worsen over several days. The intensity of the pain can fluctuate." Other symptoms can include constipation, fever, diarrhea, chills, and diverticular bleeding. Diverticular bleeding can lead to red or maroon-colored blood in the stool and can also prompt cramps, dizziness, light-headedness, and/or weakness.The cause of diverticular disease is unknown. A low-fiber diet has been linked to incidences of diverticular disease, but a concrete causal relationship has not been established. The National Institute of Diabetes and Digestive and Kidney Diseases maintains, "Studies have also found links between diverticular disease and obesity, lack of exercise, smoking, and certain medications including non steroidal anti-inflammatory drugs, such as aspirin, and steroids." Diverticular disease generally occurs in older adults above age 50, but has recently been cropping up in younger men as well.Celiac Disease affects the small intestine, which is damaged when the body has an immune response to gluten. People with celiac disease have an "inability to digest and absorb proteins called gluten [which are] found in wheat, rye, and barley. Celiac disease causes damage to the lining of the small intestine and prevents absorption of nutrients" (U.S. National Library of Medicine). When people with celiac disease consume something that contains gluten, their bodies destroy sections of villi in the small intestine. Villi are vital to the absorption of nutrients, pulling nutrients from the small intestine and moving them into the bloodstream. When the body cannot absorb nutrients, a person becomes malnourished, in spite of whatever s/he consumes.
Diverticular disease occurs when the diverticula become irritated, swollen, or inflamed, which in turn leads to infection (diverticulitis) or when a blood vessel in a diverticulum bursts (diverticular bleeding). When the diverticula cause neither diverticulitis nor diverticular bleeding, the condition is called diverticulosis. The symptoms of diverticulosis include bloating, cramps in the lower abdomen, or pain in the lower abdomen. The symptoms of diverticular disease can be more severe. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "People with diverticulitis may have many symptoms, the most common of which is pain in the lower left side of the abdomen. The pain is usually severe and comes on suddenly, though it can also be mild and then worsen over several days. The intensity of the pain can fluctuate." Other symptoms can include constipation, fever, diarrhea, chills, and diverticular bleeding. Diverticular bleeding can lead to red or maroon-colored blood in the stool and can also prompt cramps, dizziness, light-headedness, and/or weakness.The cause of diverticular disease is unknown. A low-fiber diet has been linked to incidences of diverticular disease, but a concrete causal relationship has not been established. The National Institute of Diabetes and Digestive and Kidney Diseases maintains, "Studies have also found links between diverticular disease and obesity, lack of exercise, smoking, and certain medications including non steroidal anti-inflammatory drugs, such as aspirin, and steroids." Diverticular disease generally occurs in older adults above age 50, but has recently been cropping up in younger men as well.Celiac Disease affects the small intestine, which is damaged when the body has an immune response to gluten. People with celiac disease have an "inability to digest and absorb proteins called gluten [which are] found in wheat, rye, and barley. Celiac disease causes damage to the lining of the small intestine and prevents absorption of nutrients" (U.S. National Library of Medicine). When people with celiac disease consume something that contains gluten, their bodies destroy sections of villi in the small intestine. Villi are vital to the absorption of nutrients, pulling nutrients from the small intestine and moving them into the bloodstream. When the body cannot absorb nutrients, a person becomes malnourished, in spite of whatever s/he consumes.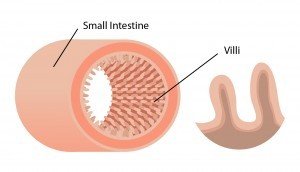 The National Institute of Diabetes and Digestive and Kidney Diseases clarifies "Celiac disease is both a disease of malabsorption—meaning nutrients are not absorbed properly—and an abnormal immune reaction to gluten." It goes by many names, including celiac disease, celiac sprue, and nontropical sprue. The symptoms of celiac disease vary widely, and some people with celiac disease may show no symptoms whatsoever. The most common symptoms of celiac disease in children include some combination of bloating, irritability, chronic diarrhea, abdominal pain, constipation, vomiting, weight loss, and "pale, foul-smelling, or fatty stool" (source). In adults, symptoms may include any of the same ones as affect children, but may also include anxiety, arthritis, bone loss, bone or joint pain, canker sores, depression, dermatitis herpetiformis (itchy rash), fatigue, infertility, iron-deficiency anemia, miscarriage, missed periods, osteoporosis, seizures, or "tingles" in the hands or feet.Approximately 1 in every 141 people has celiac disease, a genetic disorder that is now considered somewhat common. Your chances of getting celiac disease increase if you have a relative with the disease, or if you have other genetic disorders like Down syndrome or Turner syndrome.
The National Institute of Diabetes and Digestive and Kidney Diseases clarifies "Celiac disease is both a disease of malabsorption—meaning nutrients are not absorbed properly—and an abnormal immune reaction to gluten." It goes by many names, including celiac disease, celiac sprue, and nontropical sprue. The symptoms of celiac disease vary widely, and some people with celiac disease may show no symptoms whatsoever. The most common symptoms of celiac disease in children include some combination of bloating, irritability, chronic diarrhea, abdominal pain, constipation, vomiting, weight loss, and "pale, foul-smelling, or fatty stool" (source). In adults, symptoms may include any of the same ones as affect children, but may also include anxiety, arthritis, bone loss, bone or joint pain, canker sores, depression, dermatitis herpetiformis (itchy rash), fatigue, infertility, iron-deficiency anemia, miscarriage, missed periods, osteoporosis, seizures, or "tingles" in the hands or feet.Approximately 1 in every 141 people has celiac disease, a genetic disorder that is now considered somewhat common. Your chances of getting celiac disease increase if you have a relative with the disease, or if you have other genetic disorders like Down syndrome or Turner syndrome. Crohn's Disease is caused by chronic inflammation and can affect any part of the gastrointestinal tract, from the mouth to the anus. It most commonly occurs in the small intestine and in the front of the large intestine. (This disease is an inflammatory bowel disease. Other inflammatory bowel diseases include ulcerative colitis and microscopic colitis). People who get Crohn's disease are typically between the ages of 13 and 30, and it appears to run in some families. The cause of Crohn's disease is unknown, though there is speculation that it is some sort of abnormal immune response, somehow connected to genes, and/or a response to environmental stimuli .Crohn's disease has many symptoms, including abdominal pain and cramps, diarrhea, weight loss, anemia, loss of appetite, nausea, fever, and/or feeling tired. In terms of treatment, proper nutrition does play a role, just as it does with celiac disease. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "Good nutrition is important in the management of Crohn’s disease."Gastroesophageal Reflux Disease (GERD) is a chronic form of gastroesophageal reflux (GER). The National Digestive Diseases Information Clearinghouse explains, "Gastroesophageal reflux (GER) occurs when stomach contents flow back up into the esophagus—the muscular tube that carries food and liquids from the mouth to the stomach. […] Gastroesophageal reflux disease (GERD) is a more serious, chronic––or long lasting–– form of GER. GER that occurs more than twice a week for a few weeks could be GERD, which over time can lead to more serious health problems." When the esophagus becomes weak or relaxes when it shouldn't, then the stomach contents go where they shouldn't, and this can cause great discomfort. If this process happens regularly, more serious complications can occur.
Crohn's Disease is caused by chronic inflammation and can affect any part of the gastrointestinal tract, from the mouth to the anus. It most commonly occurs in the small intestine and in the front of the large intestine. (This disease is an inflammatory bowel disease. Other inflammatory bowel diseases include ulcerative colitis and microscopic colitis). People who get Crohn's disease are typically between the ages of 13 and 30, and it appears to run in some families. The cause of Crohn's disease is unknown, though there is speculation that it is some sort of abnormal immune response, somehow connected to genes, and/or a response to environmental stimuli .Crohn's disease has many symptoms, including abdominal pain and cramps, diarrhea, weight loss, anemia, loss of appetite, nausea, fever, and/or feeling tired. In terms of treatment, proper nutrition does play a role, just as it does with celiac disease. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "Good nutrition is important in the management of Crohn’s disease."Gastroesophageal Reflux Disease (GERD) is a chronic form of gastroesophageal reflux (GER). The National Digestive Diseases Information Clearinghouse explains, "Gastroesophageal reflux (GER) occurs when stomach contents flow back up into the esophagus—the muscular tube that carries food and liquids from the mouth to the stomach. […] Gastroesophageal reflux disease (GERD) is a more serious, chronic––or long lasting–– form of GER. GER that occurs more than twice a week for a few weeks could be GERD, which over time can lead to more serious health problems." When the esophagus becomes weak or relaxes when it shouldn't, then the stomach contents go where they shouldn't, and this can cause great discomfort. If this process happens regularly, more serious complications can occur. The most common symptom of GERD is heartburn, though there have been cases where people don't feel heartburn at all and instead get a dry, hacking cough. Other symptoms can include nausea after eating, feeling like food is stuck behind the breastbone, difficulty swallowing, hiccups, vomiting, asthma, wheezing, sore throat, hoarseness or vocal changes, recurrent pneumonia, chest pain, or dental erosion. Anyone can develop GERD, though if you are overweight, obese, pregnant, or a smoker, you are more likely to develop it. Certain medications can also prompt GERD. To help prevent or ease the symptoms of GERD, the U.S. National Library of Medicine advises, "Avoiding alcohol and spicy, fatty or acidic foods that trigger heartburn, eating smaller meals, not eating close to bedtime, losing weight if needed, [and] wearing loose-fitting clothes." The National Institute of Diabetes and Digestive and Kidney Diseases offers further advice, asserting "You can prevent or relieve your symptoms from gastroesophageal reflux (GER) or gastroesophageal reflux disease (GERD) by changing your diet. You may need to avoid certain foods and drinks that make your symptoms worse. Other dietary changes that can help reduce your symptoms include decreasing fatty foods [and] eating small, frequent meals instead of three large meals."Ulcerative Colitis affects the inner lining of the large intestine, usually the rectum and colon. It is a chronic condition that causes inflammation and sores -- also known as ulcers -- to develop. This inhibits the absorption of fluid and nutrients and can cause rectal bleeding and inflammation in other parts of the body. Ulcerative colitis is another inflammatory bowel disease. The other most common inflammatory bowel disease is Crohn's disease, which we explored above. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "The exact cause of ulcerative colitis is unknown. Researchers believe that factors such as an overactive intestinal immune system, genes, and environment may play a role in causing ulcerative colitis." Ulcerative colitis can strike at any age, but it is most likely to begin between the ages of 15 and 30. If you are between those ages or older than 60, or if you have a family member with ulcerative colitis, microscopic colitis, or Crohn's disease, or are of Jewish descent, your risk of getting ulcerative colitis is higher. The most typical symptoms of ulcerative colitis are abdominal pain and stool with blood or pus in it. The U.S. National Library of Medicine has laid out the less common symptoms of ulcerative colitis. They include, "anemia, severe tiredness, weight loss, loss of appetite, bleeding from the rectum, sores on the skin, joint pain [and] growth failure in children." Ulcerative colitis goes by many names and can also be called colitis, distal colitis, pancolitis, or ulcerative proctititis, depending on where the inflammation occurs.So there you have it. A closer look at 5 different digestive diseases. If you'd like to learn more, check out the links below...For More Information:
The most common symptom of GERD is heartburn, though there have been cases where people don't feel heartburn at all and instead get a dry, hacking cough. Other symptoms can include nausea after eating, feeling like food is stuck behind the breastbone, difficulty swallowing, hiccups, vomiting, asthma, wheezing, sore throat, hoarseness or vocal changes, recurrent pneumonia, chest pain, or dental erosion. Anyone can develop GERD, though if you are overweight, obese, pregnant, or a smoker, you are more likely to develop it. Certain medications can also prompt GERD. To help prevent or ease the symptoms of GERD, the U.S. National Library of Medicine advises, "Avoiding alcohol and spicy, fatty or acidic foods that trigger heartburn, eating smaller meals, not eating close to bedtime, losing weight if needed, [and] wearing loose-fitting clothes." The National Institute of Diabetes and Digestive and Kidney Diseases offers further advice, asserting "You can prevent or relieve your symptoms from gastroesophageal reflux (GER) or gastroesophageal reflux disease (GERD) by changing your diet. You may need to avoid certain foods and drinks that make your symptoms worse. Other dietary changes that can help reduce your symptoms include decreasing fatty foods [and] eating small, frequent meals instead of three large meals."Ulcerative Colitis affects the inner lining of the large intestine, usually the rectum and colon. It is a chronic condition that causes inflammation and sores -- also known as ulcers -- to develop. This inhibits the absorption of fluid and nutrients and can cause rectal bleeding and inflammation in other parts of the body. Ulcerative colitis is another inflammatory bowel disease. The other most common inflammatory bowel disease is Crohn's disease, which we explored above. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "The exact cause of ulcerative colitis is unknown. Researchers believe that factors such as an overactive intestinal immune system, genes, and environment may play a role in causing ulcerative colitis." Ulcerative colitis can strike at any age, but it is most likely to begin between the ages of 15 and 30. If you are between those ages or older than 60, or if you have a family member with ulcerative colitis, microscopic colitis, or Crohn's disease, or are of Jewish descent, your risk of getting ulcerative colitis is higher. The most typical symptoms of ulcerative colitis are abdominal pain and stool with blood or pus in it. The U.S. National Library of Medicine has laid out the less common symptoms of ulcerative colitis. They include, "anemia, severe tiredness, weight loss, loss of appetite, bleeding from the rectum, sores on the skin, joint pain [and] growth failure in children." Ulcerative colitis goes by many names and can also be called colitis, distal colitis, pancolitis, or ulcerative proctititis, depending on where the inflammation occurs.So there you have it. A closer look at 5 different digestive diseases. If you'd like to learn more, check out the links below...For More Information:
- Digestive Diseases from A-Z from the National Institute of Diabetes and Digestive and Kidney Diseases
- Celiac Disease from the National Institute of Diabetes and Digestive and Kidney Diseases
- Celiac Disease from the U.S. National Library of Medicine
- Celiac Disease Awareness Campaign from the National Institutes of Health
- Crohn's Disease from the National Institute of Diabetes and Digestive and Kidney Diseases
- Crohn's Disease from the U.S. National Library of Medicine
- Definition and Facts for Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD) from the National Institute of Diabetes and Digestive and Kidney Diseases
- Diverticular Disease from the National Institute of Diabetes and Digestive and Kidney Diseases
- Eating, Diet, and Nutrition for Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD) from the National Institute of Diabetes and Digestive and Kidney Diseases
- Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD) in Adults from the National Digestive Diseases Information Clearinghouse
- Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD) in Adults from the National Institute of Diabetes and Digestive and Kidney Diseases
- Gastroesophageal Reflux Disease from the U.S. National Library of Medicine
- Ulcerative Colitis from the National Institute of Diabetes and Digestive and Kidney Diseases
- Ulcerative Colitis from the U.S. National Library of Medicine
But wait, there's more! Here's a free handout with an overview of all 5 digestive diseases we talked about today, along with a closer look at great sources for more information. Get your copy now!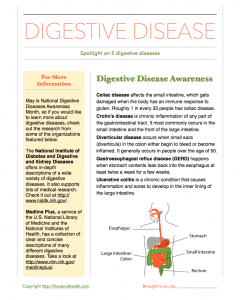 This post was brought to you by the Nutrition Education Store. For other materials and resources for National Digestive Diseases Awareness Month, check out the options below...
This post was brought to you by the Nutrition Education Store. For other materials and resources for National Digestive Diseases Awareness Month, check out the options below...