Dietary Cholesterol Promotes CVD and Total Mortality
The 2015 US Dietary Guidelines (USDG) dropped any limit on dietary cholesterol intake (1). This resulted in a change in dietary advice from those who used the USDG decision to drop limits on dietary cholesterol, which has been good for America’s egg industry but is unlikely to be good for the arteries or longevity of Americans. The American Egg Board may have made the issue more confusing with their Egg Nutrition Council newsletter. The decision to discontinue the long-standing prior advice for all Americans to limit their intake of dietary cholesterol started with a group of experts called the Dietary Guidelines Advisory Committee (DAGC). USDG basically adopted verbatim the recommendations of the panel of experts from the DAGC. The dubious advice in the proposed DAGC Report was criticized and some of the critics wrote to the DAGC explaining why the decision to drop any limit on dietary cholesterol was inconsistent with the preponderance of the most credible research on the effects of dietary cholesterol on blood lipids, cardiovascular disease (CVD). Instead, the DAGC relied on recent observational data with serious design flaws and ignored far more rigorous research from controlled clinical trials showing that dietary cholesterol adversely alters blood lipids in ways known to promote CVD. My concerns and those of other researchers about the DAGC’s Report were pretty much ignored and the DAGC’s conclusions about dietary cholesterol ended up in the USDG. I summarized my concerns about in effect telling all Americans to not concern themselves with dietary cholesterol any more here.Controlled Clinical Trials Prove Dietary Cholesterol Raises LDL-COne study that fed either 3 egg whites or 3 whole eggs daily to two groups of healthy young men for 15 days showed significant changes to their fasting and postprandial blood lipid levels. Except for the variation in egg consumption, both groups of young men were consuming the same foods. Their meals were prepared daily by the University of São Paulo and, except for the eggs, were consistent with the healthier dietary practices being advocated by the 2015 DAGC report. The diet was also low in saturated fat but high in a variety of whole foods like fruits, green vegetables, beans, chicken, and fish. Dr. Thais Cesar and colleagues reported that among the men in the group eating 3 egg whites daily, total intake of dietary cholesterol averaged only 174 milligrams per day. By contrast, among the men eating 3 whole eggs daily, daily dietary cholesterol intake averaged a whopping 804 milligrams. Dr. Cesar concluded: “A high-cholesterol diet clearly enhances LDL cholesterol levels.” At the end of the study, the egg white eaters had average LDL levels of only 86 mg/dl, while the average LDL levels for the group consuming the whole eggs was 120 mg/dl. This large daily increase in dietary cholesterol significantly increased blood cholesterol levels. On average, LDL cholesterol levels were nearly 40% higher in subjects consuming 3 whole eggs relative to those consuming only 3 egg whites (2).Dr. Mattson’s classic study proved beyond any doubt that increasing dietary cholesterol while holding other dietary variables constant results in increasing serum cholesterol levels. Figure 1 shows that increasing dietary cholesterol from zero to about 1000mg of cholesterol daily increases total serum cholesterol from about 160 to 200mg/dl or about 25% in healthy young men: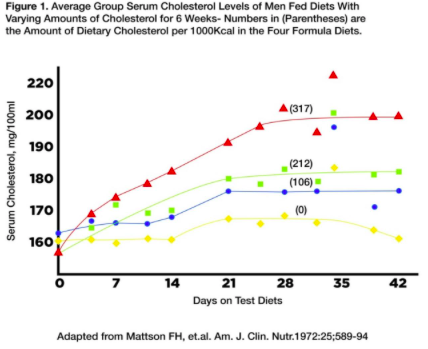 However, the DAGC and USDG ignored all this older data from well-designed and tightly-controlled clinical trials. While this older research was inconsistent with the less-questionable observational study data, it did unequivocally show that dietary cholesterol increases serum total-C and LDL-C levels far more than observational and less-tightly controlled clinical trials have been predicting. Given the difficulty of measuring dietary cholesterol accurately over many years and the propensity of those concerned about their heart artery health to limit dietary cholesterol based on longstanding advice which creates statistical noise and confounding (called reverse causation) this makes it much more difficult to show whether dietary cholesterol actually impacts the risk of CVD or total mortality in observational studies.Enter Dr. Victor Zhong at the Department of Preventative Medicine at North Western University’s Feinberg School of Medicine.Dr. Zhong and colleagues re-examined data from 20 community based prospective cohorts of US participants primarily for the study of long-term risks and development patterns of CVD over the life course in adults with an average age of 51.6 years and an average follow up of 17.5 years. Unlike many of the prior observational studies used by the DAGC, Dr. Zhong’s group selected studies involving about 30,000 subjects whose dietary intake of cholesterol was tracked over a long time and was measured as accurately as feasible in free living subjects. Given the quality data used and Dr. Zhong’s team careful statistical adjustments for confounding dietary variables the results of this new study seriously undermine whatever credibility the 2015 USDG may have had.Dr. Zhong Shows Dietary Cholesterol Increases Risk of DeathThe new research by Dr. Zhong showed a significant association between increasing dietary cholesterol consumption with an increased risk of incident CVD and all-cause mortality. These adverse effects were shown to be independent of fat intake with neither the amount of fat and/or the quality of dietary fat affecting the significant association between higher dietary cholesterol intake and elevated risk of CVD and total mortality. These findings are consistent with prior evidence that had shown a reduction of dietary cholesterol intake, as well as isocaloric replacement of saturated fat by unsaturated fat, were both significantly associated with a reduction in total cholesterol (primarily LDL-cholesterol) concentration. Given the strong and consistent association between elevated total and LDL cholesterol levels and increased risk of more coronary artery disease and more deaths from heart disease, it would be surprising if more dietary cholesterol did not increase the risk of CVD events and total mortality.Dr Zhong’s data demonstrated the significant association between egg consumption and incident CVD was fully accounted for by the cholesterol content in eggs, which also largely explained the significant association between egg consumption and all-cause mortality. This offered additional support for the significant associations between dietary cholesterol consumption with incident CVD and all-cause mortality. Egg consumption contributed about 25% to the total dietary cholesterol consumed and meat consumption contributed about 42%. Mechanically, eggs and processed or unprocessed red meat are rich in other nutrients such as choline, iron, carnitine, and added sodium (for processed meat) that may also be involved in CVD risk via different pathways. Finally, it should be noted that Dr. Zhong’s data showed that the significant associations of dietary cholesterol or egg consumption with more CVD events and increased all-cause mortality were similar between participants who consumed a higher quality diet and those who consumed a more typical modern diet. This observation suggests that people may need to minimize dietary cholesterol and egg yolk intake even if they are following a healthier eating pattern such as a Mediterranean-style diet or a DASH-type diet, which are now being recommended by the Institute of Medicine.Bottom Line: Given that Dr. Zhong’s study is now the best quality data we have on the health and longevity effects associated with dietary cholesterol intake, it seems likely that the 2020 USDG will have little choice but to resume recommending that all Americans (and not just those with CVD) ought to be advised to limit their dietary cholesterol intake. Of course, this flip flopping will be used by the egg, meat, and animal product industry to sow confusion and undermine the credibility of the USDG. Sadly for the USDG and their expert committees, their willingness to cater to the commercial interests of the animal foods and especially the egg industry has probably cost them some credibility. They should never have ignored earlier data showing, at the very least, that more dietary cholesterol leads to higher serum cholesterol and LDL-C, which we have long known promotes more CVD and increases the risk of death. Until those new dietary guidelines come out, it would be wise to point out the errors made by the last DAGC and the USDG to patients and clients who have been misled into believing that dietary cholesterol is no longer something they should be concerned with. Increasing dietary cholesterol leads to more CVD and greater risk of dying.By James J. Kenney, PhD, FACNReferences:
However, the DAGC and USDG ignored all this older data from well-designed and tightly-controlled clinical trials. While this older research was inconsistent with the less-questionable observational study data, it did unequivocally show that dietary cholesterol increases serum total-C and LDL-C levels far more than observational and less-tightly controlled clinical trials have been predicting. Given the difficulty of measuring dietary cholesterol accurately over many years and the propensity of those concerned about their heart artery health to limit dietary cholesterol based on longstanding advice which creates statistical noise and confounding (called reverse causation) this makes it much more difficult to show whether dietary cholesterol actually impacts the risk of CVD or total mortality in observational studies.Enter Dr. Victor Zhong at the Department of Preventative Medicine at North Western University’s Feinberg School of Medicine.Dr. Zhong and colleagues re-examined data from 20 community based prospective cohorts of US participants primarily for the study of long-term risks and development patterns of CVD over the life course in adults with an average age of 51.6 years and an average follow up of 17.5 years. Unlike many of the prior observational studies used by the DAGC, Dr. Zhong’s group selected studies involving about 30,000 subjects whose dietary intake of cholesterol was tracked over a long time and was measured as accurately as feasible in free living subjects. Given the quality data used and Dr. Zhong’s team careful statistical adjustments for confounding dietary variables the results of this new study seriously undermine whatever credibility the 2015 USDG may have had.Dr. Zhong Shows Dietary Cholesterol Increases Risk of DeathThe new research by Dr. Zhong showed a significant association between increasing dietary cholesterol consumption with an increased risk of incident CVD and all-cause mortality. These adverse effects were shown to be independent of fat intake with neither the amount of fat and/or the quality of dietary fat affecting the significant association between higher dietary cholesterol intake and elevated risk of CVD and total mortality. These findings are consistent with prior evidence that had shown a reduction of dietary cholesterol intake, as well as isocaloric replacement of saturated fat by unsaturated fat, were both significantly associated with a reduction in total cholesterol (primarily LDL-cholesterol) concentration. Given the strong and consistent association between elevated total and LDL cholesterol levels and increased risk of more coronary artery disease and more deaths from heart disease, it would be surprising if more dietary cholesterol did not increase the risk of CVD events and total mortality.Dr Zhong’s data demonstrated the significant association between egg consumption and incident CVD was fully accounted for by the cholesterol content in eggs, which also largely explained the significant association between egg consumption and all-cause mortality. This offered additional support for the significant associations between dietary cholesterol consumption with incident CVD and all-cause mortality. Egg consumption contributed about 25% to the total dietary cholesterol consumed and meat consumption contributed about 42%. Mechanically, eggs and processed or unprocessed red meat are rich in other nutrients such as choline, iron, carnitine, and added sodium (for processed meat) that may also be involved in CVD risk via different pathways. Finally, it should be noted that Dr. Zhong’s data showed that the significant associations of dietary cholesterol or egg consumption with more CVD events and increased all-cause mortality were similar between participants who consumed a higher quality diet and those who consumed a more typical modern diet. This observation suggests that people may need to minimize dietary cholesterol and egg yolk intake even if they are following a healthier eating pattern such as a Mediterranean-style diet or a DASH-type diet, which are now being recommended by the Institute of Medicine.Bottom Line: Given that Dr. Zhong’s study is now the best quality data we have on the health and longevity effects associated with dietary cholesterol intake, it seems likely that the 2020 USDG will have little choice but to resume recommending that all Americans (and not just those with CVD) ought to be advised to limit their dietary cholesterol intake. Of course, this flip flopping will be used by the egg, meat, and animal product industry to sow confusion and undermine the credibility of the USDG. Sadly for the USDG and their expert committees, their willingness to cater to the commercial interests of the animal foods and especially the egg industry has probably cost them some credibility. They should never have ignored earlier data showing, at the very least, that more dietary cholesterol leads to higher serum cholesterol and LDL-C, which we have long known promotes more CVD and increases the risk of death. Until those new dietary guidelines come out, it would be wise to point out the errors made by the last DAGC and the USDG to patients and clients who have been misled into believing that dietary cholesterol is no longer something they should be concerned with. Increasing dietary cholesterol leads to more CVD and greater risk of dying.By James J. Kenney, PhD, FACNReferences:
- https://health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf
- http://jn.nutrition.org/content/136/4/971.full or https://academic.oup.com/jn/article/136/4/971/4664326


